13 hours ago
By David Cox,Features correspondent
 Getty Images
Getty Images
The winter vomiting bug is highly infectious and fast to evolve, but can we learn anything from groups of people who are unusually immune to the virus?
When it comes to surviving in the environment, few pathogens are more resilient than norovirus. This gastrointestinal bug induces nasty bouts of diarrhoea and vomiting in around 685 million people globally every year, often in hospitals, nursing homes, jails, schools and cruise ships.
The latest statistics from the Centers for Disease Control and Prevention reveal that the germ is spreading rapidly once again across the US, with cases climbing particularly quickly since October 2023 in the northeast of the US.
But to understand why norovirus is so hard to stop once an outbreak gets going, you first have to appreciate just how much it can endure. "It's a very tough little virus," says Patricia Foster, professor emerita of biology at Indiana University Bloomington who has studied norovirus. The virus is able, for example, to survive intact within food up to temperatures of 70C (158F). "It can survive heat, freezing cold, extreme dryness, and so it just sits on surfaces for days," says Foster.
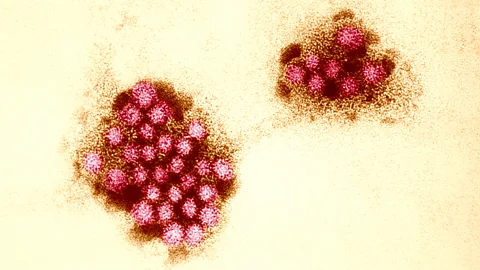
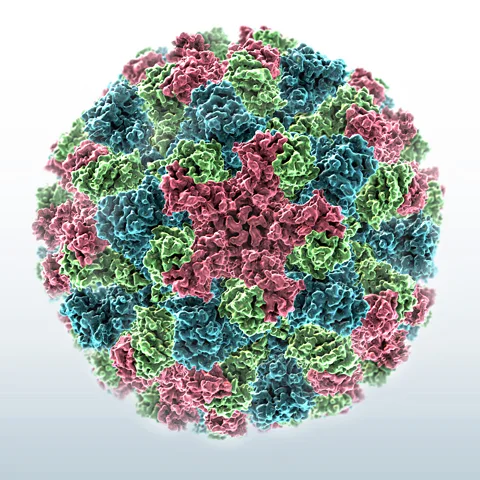
Much of this toughness comes down to the surface of the virus, a protein coat which acts a little like armour, shielding its inner genetic material. Foster points out that while a lot of viruses acquire a membrane coat as they pass from cell to cell, facilitating their ability to spread within the body, this also makes them susceptible to alcohol and detergents.
"Norovirus doesn't do that," she says. "It's just a little protein bomb, and so things like hand sanitiser can't kill it, while it's still able to move from cell to cell."
 Alamy
Alamy
The surface proteins that make up the outer coat of norovirus act like a suit of armour, meaning it can be tough to kill (Credit: Alamy)
We still understand relatively little about exactly how norovirus spreads within the body, but we do know that it spreads between people remarkably quickly. It is thought to take as little as 10 norovirus particles for an infection to take hold, while in comparison, it has been estimated that the so-called infective dose for Covid-19 is in the region of 100-400 units of the SARS-CoV-2 virus.
However, in recent decades virologists have begun to discover that there are some of us who carry innate biological factors which protect us from the illness.
So-called "challenge studies" where paid volunteers agree to be deliberately infected with a norovirus strain, have helped determine that as many as one in five people of European descent carry a mutation in a gene called FUT2. This inactivates an enzyme that protects them against GII-4, the most common of the 29 norovirus strains currently known to be capable of infecting humans and responsible for causing 50 to 70% of all norovirus outbreaks in the world.
The reason for this is because norovirus largely prefers to enter the cells in the small intestine via antigens, molecular gateways called oligosaccharides, which are made from an assortment of different sugars. Both GII-4 and many other norovirus strains require one particular oligosaccharide, called the H1-antigen, in order to infect a person.
But people carrying a mutation in the FUT2 gene lack an enzyme that is involved in a vital step in the formation of the H1-antigen in mucous producing cells in the mouth, throat, gut and lungs. Without these antigens on their cells, the GII-4 virus is unable to cause an infection. As people who carry this mutation don't produce the FUT2 enzyme in mucous-producing cells, they are known to virologists as non-sectors.
For the same reason, your blood type, something which is determined by your genetic makeup, also plays a large role in resistance and susceptibility to different norovirus strains. People with B blood type tend to be more resistant as fewer strains have evolved to attach to those particular oligosaccharides, whereas those with A, AB or O blood types are far more likely to become sick.
It means you're somewhat resistant but not completely, as norovirus evolves extremely rapidly – Patricia Foster
According to Robert Atmar, a virus expert and professor at Baylor College of Medicine in Houston, Texas, this information could in future aid the development of better antivirals against norovirus strains. "There are studies being done to see if taking advantage of the interaction between noroviruses and the antigens on cells might be targeted for the development of a therapeutic," he says.
However, this work is complex because of the speed with which noroviruses adapt and change their genetic material, meaning that some strains have still found a pathway to infect individuals who are relatively resistant.
You might also like:
"I'm a non-secretor myself," says Foster. "It means you're somewhat resistant but not completely, as norovirus evolves extremely rapidly."
She predicts that even non-secretors may become more susceptible to variants of GII-4 with time, as this strain of norovirus figures out different pathways into the body.
"I was reading about the evolution of GII-4 and all the variants that have appeared over the last 20 years or so, mostly in China," she says. "They find that it's getting better and better at interacting with different binding sites on our cells. So that's the evolution game."
While norovirus doesn't tend to kill its host, it can prove lethal to anyone with a weakened immune system, children, and the elderly. It results in around 200,000 deaths every year, particularly in low-income countries, but also 70,000 hospitalisations in the US. As a result, virologists are now trying to utilise our growing knowledge about the virus to help design vaccines.

 Getty Images
Getty Images
Norovirus outbreaks can be particularly serious on cruise ships, where infections can spread rapidly (Credit: Getty Images)
The vaccine scourge
For decades, norovirus has been devilishly difficult to even contemplate vaccinating against. One of the most problematic reasons is that the noroviruses evolve so rapidly, it means any vaccines are quickly out of date. Human norovirus is also notoriously difficult to grow in the laboratory, making it difficult to study.
However, in the last few years, researchers have begun to devise ways of growing the virus within human gut cells in a petri dish, something which could prove invaluable in testing the best way to induce a suitably powerful antibody response from the immune system.
"These cell culture models may be helpful in vaccine efforts by demonstrating that immune responses generated after vaccination kill or inactivate the virus by neutralising its infectivity," says Atmar.
But because there are so many norovirus strains and a seemingly continuous flow of new variants, a vaccine will need to induce a very broad immune response. Ming Tan, an associate professor in infectious diseases at Cincinnati Children's Hospital Medical Center, Ohio, says that a so-called bivalent or multivalent vaccine, which contains multiple immune-driving particles from various points in the virus' genetic code, will almost certainly be necessary to achieve any chance of durable immunity.
Having such a vaccine is likely to be particularly important if it is rolled out in young children to prevent a phenomenon known as "immune imprinting". This is the tendency of the immune system to misidentify a new viral variant as one it has already encountered, thus mounting an ineffective antibody response. Researchers at the University of North Carolina believe that if a suitably broad norovirus vaccine is administered to children who are around six months old, the jab could then guide the antibody response to any further variants.
Developing a broad vaccine is not an easy task, but multiple companies and research groups have taken on the challenge, each choosing to utilise different technological platforms. Moderna have launched a clinical trial of a messenger RNA (mRNA) norovirus vaccine initially in 18-49 year olds and 60-80 year olds. Meanwhile, Boston-based biotech HilleVax is conducting trials of its vaccine candidate in five-month-old infants, children aged two to nine, adults aged 18-59 and over 60s. HilleVax's approach is to use virus-like particles (VLPs), molecules which mimic norovirus strains and so trigger an immune response, without actually being infectious.
"We're still learning a lot about norovirus vaccines and how they might protect," says Atmar. "We know that administration of virus-like particle (VLP)-based vaccines via the nose or by intramuscular injection can lead to protection from illness. mRNA vaccines may allow increased numbers of strains to be included. I think all will likely be effective, and the relative effectiveness will depend on other factors we are still learning about, including breadth of the immune response after vaccination, duration of immune response, and role of past infection and genetic makeup on an individual's response and protection."

 Getty Images
Getty Images
Advances in mRNA vaccines are raising hopes of being able to inoculate against noroviruses (Credit: Getty Images)
Yet for all these efforts, success will also likely depend on how swiftly the vaccine needs to be updated and re-administered as a booster jab. Tan, who recently published a study on his own laboratory's approach to a norovirus vaccine, admits that this could be a hurdle.
"Vaccines produced using our approach will need regular updates to address the challenges of rapid virus evolution and the potential emergence of new norovirus genotypes as predominant strains in the future," he says.
However, Atmar remains more optimistic, saying that we need to wait until the results of much larger trials before any firm conclusions can be made on potential vaccine durability.
"The results of one of the studies for the VLP vaccine being pursued by HilleVax suggests that it can also protect against disease caused by the GII-2 strain when the vaccine contained GI-1 and GII-4 strains," he says. "So, we don't know whether it'll be like influenza or Covid [where regular boosters are required], or that it might be more like RSV where strain updates are not needed."
But if we can develop at least one vaccine in the years to come, it will represent a major step forward in humanity's ongoing battle with norovirus.
"We've been evolving in parallel with this virus for hundreds of thousands of years," says Foster. "And it can be a killer, particularly for babies and people who are immunocompromised because they can't rid themselves of the virus, so any vaccine would be progress."
--
If you liked this story, sign up for The Essential List newsletter – a handpicked selection of features, videos and can't-miss news delivered to your inbox every Friday.